Equine/Horse Canker
Equine/Horse Canker: Who, Where, and Early Signs
Equine/Horse Canker: What Is In Horse Canker Powder
Equine/Horse Canker: Confusion That It’s Thrush
Equine/Horse Canker: Causes of Canker
Equine/Horse Canker: Why It Can Occur At Even Well Managed Barns
Equine/Horse Canker: Role of Worms
Equine/Horse Canker: Prevention
Equine/Horse Canker: Treatments That Do Not Work
Equine/Horse Canker: Euthanasia
Equine/Horse Canker: Studies
Equine/Horse Canker: Role of Metronidazole
Equine/Horse Canker: Role of Tetracycline Treatment
Equine/Horse Canker: Role of Treponema Spirochete
Equine/Horse Canker: Role of Bovine Papillomavirus
Equine/Horse Canker: Using Ketaconazole
Equine/Horse Canker: Biopsy and Lab Testing Canker, Why Take X-Rays of Foot
A. Equine/Horse Canker: Who, Where, and Early Signs
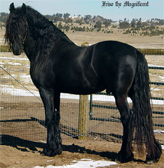
1. All breeds are effected by canker, but draft/draft crosses seem to have a higher rate
2. All ages and sexes can get it
3. Can be in one, two, three, or all four feet:
In drafts, it is usually more in the hind feet
4. Early Signs:
a. Very bad odor
b. Exudate that is white/yellow like melting cheese
c. Tentacles of abnormal tissue like an octopus (in advanced cases)
e. “Blooms” of proud flesh and abnormal tissue that looks like cauliflower
f. Tissue bleeds very easily when trying to clean out the feet
Cleaning out feet does not cure the problem
g. Mild advancing to profound lameness where they begin to lean against posts,straw bales, keep feet up, hop, toe walk
h. Blood on concrete floor seen due to canker dripping blood
5. Your farrier says the horse has canker
B. Equine/Horse Canker: What is in Horse Canker Powder?
A proprietary blend of desiccants, antibacterials, antifungals, vitamins, herbs and anti-inflammatory agents:
1. MSM
2. Matricaria
3. Magnesia desiccant
4. Metronidazole
5. Ketoconazole
6. SMZ/TP
7. Vitamin E
The 1 gallon bucket is enough to treat 2 feet for 4 weeks to clear horse canker.
![]() Click here for Canker Powder Protocol
Click here for Canker Powder Protocol
C. Equine/Horse Canker: Confusion That It’s Thrush
A. Differences
| Canker | Thrush | |
| Where? | All over body of frog, sole | Only sulcus (grooves) of the frog – not the body, not sole |
| Proliferate Tissue? | Yes, large amounts of proud flesh or even tentacles of abnormal tissue | No |
| Color of Exudate | Yellow, white melting cheese-like | Usually black |
| Time to heal | 3-4 weeks | 1 week |
| Common | No | Yes |
| Oral antibiotics used | Yes | No |
| Spirochete Aspect | Yes | No |
| Bleeds easily | Yes | No |
| Viral Aspect | Yes | No |
| Worm Aspect | Yes | No |
B. Similarities
1. Both have a bad odor
2. Both improve with dry bedding/dry turnout areas
3. Both improve with picking out feet regularly
D. Equine/Horse Canker: Causes of Canker
These pile up on each other to create the disease – so it’s a “soup” of causes all mixed in, with the percent of each trigger different in each case.
1. Viral – bovine papilloma virus
2. Bacterial – anaerobes, including Treponema Spirochete
3. Bacterial – aerobes
4. Proliferative abnormal tissue – proud flesh/hyperkeratosis, hyperplastic tissue
5. Fungal elements probable
6. Nematode (worms) probable
E. Equine/Horse Canker: Why It Can Occur At Even Well Managed Barns
1. Treponema in soil is worldwide
2. Bovine papilloma virus is widespread
3. Peloda worms in soil is worldwide
4. Bedding in straw increases infection possibility due to organic matter being in direct contact with dirt. Also straw absorbs urine less, so more moisture allows for increased bacterial counts.
5. Genetic component – horse may be more prone
6. Drafts more prone – perhaps weight pushes dirt into crevices in foot in larger amounts. Perhaps larger foot means more prone to frog/sole wounds which allow dirt in more often.
F. Equine/Horse Canker: Role of Worms
Worms (nematodes) as an agent of horse canker
![]() Click here to see Dr. Raven’s article on papillomatous dermatitis in a Tennessee Walking Horse
Click here to see Dr. Raven’s article on papillomatous dermatitis in a Tennessee Walking Horse
1. Tennessee walking horse with Horse papillomatous dermatitis had spirochetes and the worm pelodara strongyloides within the abnormal tissue
2. This worm is a saprophyte – it lives in dead or decomposing organic material
3. The area had classic epidermal hyperplasia and keratotic hyperkeratosis
4. Antibiotics were used to treat the spirochetes – tetracycline class
5. Pelodera strongyloids diagnosed also in humans, dogs, cattle, and horses
![]() Click here to see an article by the CDC on strongyloides
Click here to see an article by the CDC on strongyloides
1. In humans, pelodara strongyloids creates an itchy, red, rash
2. First line of therapy is Ivermectin given to people
![]() Click here to see Dr. Naquira’s article on Ivermectin use from Human Strongyloides
Click here to see Dr. Naquira’s article on Ivermectin use from Human Strongyloides
1. Ivermectin in people helped strongyloidiasis
2. 88% cure rate with Ivermectin
3. Well tolerated
![]() Click here to see Dr. Kohler’s article on the effectiveness of Ivermectin
Click here to see Dr. Kohler’s article on the effectiveness of Ivermectin
Ivermectin used to treat equine strongyloides – strongyloids westeri in foals with “high efficacy and no side effects”
![]() Click here to see Dr. Saari’s article strongyloides as a cause of dermatitis in dogs
Click here to see Dr. Saari’s article strongyloides as a cause of dermatitis in dogs
1. Pelodera strongyloides seen in dogs on damp ground or damp bedded straw. This is a good reason to avoid straw as bedding in horses – use shavings
2. Creates inflammatory skin reaction as larvae burrow into skin
![]() Click here to see Dr. Yeruham’s article about dermatitis in a dairy herd caused by strongyloides
Click here to see Dr. Yeruham’s article about dermatitis in a dairy herd caused by strongyloides
1. High rate (25%) of a cattle herd infected with pelodara strongylades
2. Created marked thickening of skin, scurfy, and hair loss
3. A moist/filthy environment was suggested as a mechanism for infection
![]() Click here to see Dr. Tanaka’s article on strongyloid infestations being presented as dermatitis
Click here to see Dr. Tanaka’s article on strongyloid infestations being presented as dermatitis
1. Pelodera strongyloides in an 18 year old man – itchy, follicular papulopustules on skin
![]() Click here to see Dr. Ginsburg’s article on dermatitis caused by the larvae of a soil nematode
Click here to see Dr. Ginsburg’s article on dermatitis caused by the larvae of a soil nematode
1. 6-month old baby with pelodera strongyloides
CONCLUSIONS
a. Create abnormal skin/usual skin barrier is broken down to allow bacteria in
b. Live in dead/decaying organic material, so clean up any loose hay in fields, avoid straw as bedding if your horse has had canker prior
c. Use Ivermectin in the treatment regiment for horse canker. Consider using it in usual deworming program such as twice a year Equimax which has Ivermectin in it
G. Equine/Horse Canker: Prevention
Prevention of canker – being proactive:
A. Bedding
Use shavings to dry out feet better than straw. Straw has organic dust which includes bacteria/mold and absorbs urine less, so the feet are exposed to water more. Pelodara larvae live in rotting organic debris like wet straw.
B. Pick feet out daily/inspect feet daily
C. Antiseptic
Apply Venice of Turpentine to soles of all four feet 2 times a week for life – antiseptic
D. Help the Barrier
Understand that the hooves/soles are extensions of the skin, so help that barrier be its best:
1. Health-E Vitamin E: 1 scoop a day = 5,800 IU of Vitamin E. This is the strongest Vitamin E in the USA, has all eight forms of alpha tocopherol, and is ester stable so it is good for 2 years in heat/light/air. Vitamine E is the #1 antioxidant of the epidermal tissue making up frog/sole.Why Vitamin E? Keeps immune system in peak shape in studies.
![]() Click here for information on Vitamin E
Click here for information on Vitamin E
2. Omega 3 helps skin – add flax or chia seed to their diet – easy, simple, and cheap
E. Pasture
Management of pasture to decrease area of standing water
F. Genetic Component
Family lines of an individual horse with canker need to be inspected daily even more. If a canker horse has a brother on the program, a keep a sharp eye on them.
G. Deworming
Regular deworming program reduce the nematode aspect of canker – do Ivermectin 3x per year
H. Avoid Long Term Corticosteroid Use
Lowers immune system to allow bacteria in
H. Equine/Horse Canker: Treatments That Do Not Work
1. Caustic Chemicals
These can destroy normal tissue and create crevices that canker flourish in. They can also spill over hoof tissue onto skin of the heels/pastern and create damage.
2. Deep/Radical Surgical Debridement with No Follow Up
These require general anesthesia, so added risk and costs, and the canker will return. Often normal tissue and structures are removed unnecessarily.
3. Maggot Therapy for Cleaning Out Necrotic Tissue
This treatment cannot reduce proud flesh aspect of canker or kill harmful bacteria of the disease. This therapy usually also requires surgical removal of some abnormal tissue prior to maggot placement. A better option is the surgical removal of abnormal tissue and placement of horse canker powder.
4. Freeze Firing
Often requires multiple separate treatments due to canker reoccurs. This therapy also requires surgical removal of canker tissue prior to the procedure and often, topicals are required after freeze firing. A quicker, easier way is surgical removal and placement of horse canker powder.
5. High Dose Oral Corticosteroids
One study suggested this to help in reducing proud flesh aspect of canker but it’s a therapy with problems:
a. Immune Suppression Caused by Steroids: This can increase bacterial infections. Also Cushings horses should avoid this due to raising of glucose levels and their cortisol levels are already high. In addition, corticosteroid reduces muscle mass by breaking it down to create glucose, so it is not helpful in older horses with muscle problems.
b. Laminitis: Increases insulin, so it is not good for insulin resistant horses and can increase laminitis episodes in IR horses.
c. Proven to create IR in normal horses with extended use.
6. Chloramphenicol Topical Antibiotic
a. Human Health Hazard. Other antibiotics like SMZ-TP, tetracyclines, metronidazole, and ketoconazole are much safer.
b. Expensive
7. The Use of Cisplatin Anti-Cancer Agent to Treat Horse Canker
A. Dr. Apprich, “Equine Hoof Canker: A Clinical Trial of Topical Cisplatin Chemotherapy”
1. In the study, a major problem was that included in with cisplatin was metronidazole – so it’s very difficult to see which medicine was having effect.
2. Of 10 horses treated, 6 out of 10 had less than 2 months of follow-up to see if it reoccurred. So, no idea what happened after that.
3. In 1 out of 10, canker did reoccur when tracked for 14 months post-treatment.
4. Due to health and safety concerns, “made this therapy viable only in a hospital setting.”
B. Dr. Florea, Cancer 2011, Cisplatin Activity/Side Effects
“Cisplatin may lead to diverse side effects such as neuro and/or renal toxicity or bone marrow-suppression”
“Despite the positive effects of platinum compounds, they are poisons”
“Cisplatin creates DNA damage to tissue – considered a DNA-damaging anticancer drug”
Due to the potential to damage normal tissue on the hoof or horse skin if split or runs accidentally onto it; and the multiple (at least 14) times you need to handle it as a veterinarian, along with the dangers to human skin and bone marrow problems, it’s wise to look for other safer treatments for horse canker. Also, this treatment cannot be done at a barn or stable – it would only be at a hospital, so costs would be much greater.
I. Equine/Horse Canker: Euthanasia
The need for past euthanasia often was due to the lack of recent knowledge that we have now. More accurate trimming of necrotic tissue, correct antibiotics, the importance of keeping dry are adding up to increased success.In the recent past, canker was often a grave prognosis:
a. 1962 – Lameness in Horses (Dr. Adams)
“Guarded to unfavorable prognosis”
b.1998 – The Lame Horse (Dr. Rooney)
“Less than hopeful prognosis”
More and more, euthanasia is not being considered due to canker getting cleared up.
J. Equine/Horse Canker: Studies
1. Dr. Evans StudyPresence of Treponema on hooves is NOT diagnostic of canker in horses.
Cattle that had PCR biopsy of skin near the hoof that were negative for treponema, still had positive PCR for for treponema on healthy hoof tissues. These cattle were brought to a farm with cattle with present cattle digital papillomatous dermatitis levels.
This means a simple culture of treponema of a horses foot will NOT mean it’s canker positive.
This also means that treponema are present in the dirt at a farm with a horse with canker most likely. Whether treponema is ubiquitous (all over) to all horse farms is unknown. Whether the load/amount of treponema at a farm contributes to more canker is unknown.
Presence of cattle digital dermatitis bears important information to consider in horse canker.
Cattle digital papillomatous dermatitis is worldwide – so is horse canker.Cattle digital dermatitis has the same treponema found in horses. Treponema denticola-like spirochetes found in diseased cattle digital dermatitis (76.5% of cases).79% of human endodontic (gum line) abscess showed PCR genetic testing also for treponema denticola.
This treponema spirochete effects many animals – humans, horses, dogs
In cattle, they isolated several species of treponema in diseased tissue – not just treponema denticola. It’s very possible more treponema species than just treponema denticola-like will be found in horse canker
2. Click here to see Dr. Yano’s study in the Journal of Clinical Microbiology (2009) on different spirochete strains that were found in cattle papillomatous digital dermatitis
In cattle papillomatous Digital Dermatitis in a Japan study, 40 different spirochete strains were found
Cattle papillomatous digital dermatitis creates hyperkeratotic papillomatous lessons with long hair like projections – this is the same thing found in horse canker
>Many different types of bacteria cultured in BPDD – unclear whether some or all involved, but a large number of spirochetes found.
Culturing out treponema in diseased tissue is a difficult process due to growth rate of treponema being poor.
Also, presence if other fast growing bacteria in lesions prevents treponema isolation. No selective growth media for these treponema has been developed
> So if culturing and have a treponema negative result, that does not mean they were NOT present.
Did find systemic antibodies against certain spirochetes in diseased tissue, so an immune response is being made, but it may not be protective or due to so many species of spirochetes, the genetic diversity is so great that it evades immunological responses to clear infection.
3. Click here to see Dr. Tanabe’s article in the Journal of Periodontal Research (2009) on treponema denticola being a key pathogen in periodontitis disease
Treponema denticola is a key pathogen in human periodontitis (gum) disease.
This spirochete creates a large inflammatory reaction to tissues around it – TNF, IL-1, IL-6, IL-8, MMP, prostaglandins are pro-inflammatory cytokines that all increased.
So in horses, it’s setting off inflammation in hoof canker tissue.
K. Equine/Horse Canker: Role of Metronidazole
Metronidazole in human periodontitis
A. Click here to see Dr. Vergani’s study (2004) on metronidazole in the treatment of chronic periodontitis
Metronidazole antibiotic indicated against certain anaerobic infection, safe in humans, widely used.
When studied between just cleaning, just metronidazole, or cleaning and metronidazole, the cleaning and metronidazole dropped infections the most – by 79% – they did not eliminate it, but there was a huge reduction.
Metronidazole treated people also had less bleeding of gums post treatment.This is why metronidazole is important in canker therapy of horses.
B. Click here to see Dr. Baehni’s article (1992) “Treponema denticola induces actin rearrangement and detachment of human gingival fibroblasts”
Treponema denticola actively detaches fibroblasts from gum tissue, leading to tissue detachment. It is actively destroying tissue – this allows other bacteria to move in.
Metronidazole helped to “markedly reduce the detachment response”.
Metronidazole helps in protecting tissues infected with spirochetes.
C. Click here to see Dr. Khodaeiani’s article in the Indian Journal of Dermatology (2012) “Efficacy of 2% metronidazole gel in moderate acne vulgaris”
Using metronidazole topically is effective and safe, even on human faces to treat acne. Had a 88% patient satisfaction and redness on face decreased by 85%.
“Found effective and safe”
D. Click here to see Dr. Jain’s evaluation of combining metronidazole and benzoyl peroxide from treatment of acne vulgaris (1998)
A study mixing metronidazole with benzoyl peroxide for acne showed good effects over an 8-week period. Again on human faces, this combination was safe.
Benzoyl peroxide is an active ingredient in Clearasil used in teen acne
Comment from Dr. Reilly: Some vets report results if they first do a surgical resection of the area, followed by Freeze Firing and then applying metronidazole/benzoyl peroxide mix
L. Equine/Horse Canker: Role of Tetracycline Treatment
Use of Tetracyclines to help in human treponema periodontitis infections
A. Click here to see Dr. Nelson’s article (2015) “Preventing and treating periodontitis”
Doxyxyxline helped – cleaning/debriding area alone did not help – need doxy added
Found that diabetes that were treated had better glycemic control. This may be of interest in IR or cushing horses – reducing infection, reducing pain of canker may help in these diseases.
B. Click here to see Dr. Schnabel’s article in the Equine Veterinary Journal (2010) “Orally administered doxycycline accumulates in synovial fluid compared to plasma”
Doxycycline can concentrate in tissues above the levels found in bloodstream.
C. Click here to see Dr. Bryant’s study in the Equine Veterinary Journal (2000) on administration of doxycycline
The correct dose of Doxycycline is 10 mg/kg body weight every 12 hours. This means in a 1,100 pound horse, the dose is 5 grams AM & 5 grams PM.
Comment from Dr. Reilly: So, foil pack of 5 grams each are easy, cheap, and helpful.
M. Equine/Horse Canker: Role of Treponema Spirochete
Treponema is a probable canker component around the world.
1. Treponema denticola-like spirochetes are also found in other parts of the world such as in the UK. PCR testing of diseased cattle Digital Dermatitis found it in 76.5% of cases
![]() Click here to see Dr. N Evans study in the Journal of Clinical Microbiology (2009) on the “Association of Unique, Isolated Treponemes with Bovine Digital Dermatitis Lesions”
Click here to see Dr. N Evans study in the Journal of Clinical Microbiology (2009) on the “Association of Unique, Isolated Treponemes with Bovine Digital Dermatitis Lesions”
2. Bovine Digital Dermatitis is a worldwide disease
N. Equine/Horse Canker: Role of Bovine Papillomavirus
Dr. Brandt 2011, Equine Veterinary Journal
1. DNA testing of horse canker showed in 24 of 24 cases of Bovine (cow) papillomavirus (BPV)
2. Viral sequencing is 98% BPV in horse canker
3. Testing of horse tissue with no signs of canker showed 13 of 13 times , no BPV
Conclusion: BPV is an active contributor to horse canker. BPV in cattle produces many of the signs seen in horses such as hyperkeratosis, acanthosis, and moist pododermatitis
1. BPV is common on the skin of normal horses, if they are around horses with sarcoids
2. BPV is common on the skin of horses with sarcoids
O. Equine/Horse Canker: Using Ketoconazole
1. Ketoconazole found to be highly effective against 40 isolates of fungus
2. Ketoconazole highly effective in vivo and in vitro
![]() Click here to see Dr. Hessen’s article on oral and topical ketoconazole in the treatment of pityriasis versicolor
Click here to see Dr. Hessen’s article on oral and topical ketoconazole in the treatment of pityriasis versicolor
3. In comparing miconazole and ketoconazole topically on skin against Candida Fungus, ketoconazole produced 14 x, 10 x, and 7 x greater drug concentrates at 1, 4, and 8 hours than did miconazole
4. Ketoconazole had significantly greater bioactivity than did miconazole
5. Ketoconazole had greater efficacy than miconazole
![]() Click here for Dr. Pershing’s article on …
Click here for Dr. Pershing’s article on …
6. Ketoconazole used against seborrheic dermatits and it improved erythema (redness), scaling, and pruritus (itch)
7. Ketoconazole reduced symptom severity 53%
8. Ketoconazole found to be effective, well-tolerated, convenient and acceptable treatment
![]() Click here to see Dr. Elewski’s article on “Efficacy and safety of a new once-daily topical ketoconazole 2% gel in the treatment of seborrheic dermatitis: a phase III trial”
Click here to see Dr. Elewski’s article on “Efficacy and safety of a new once-daily topical ketoconazole 2% gel in the treatment of seborrheic dermatitis: a phase III trial”
9. Animal studies indicate topical ketoconazole was very active in the most common skin infections10. Not reported to give dermal absorption and was not toxic to animals
![]() Click here to see Dr. Cauwenbergh’s article on “Topical Ketoconazole in Dermatology: A Pharmacological and Clinical Review”
Click here to see Dr. Cauwenbergh’s article on “Topical Ketoconazole in Dermatology: A Pharmacological and Clinical Review”
P. Equine/Horse Canker: Biopsy and Lab Testing Canker, Why Take X-Rays of Foot
Farrier Dave Giza taught me this valuable lesson in having the option to test a hunk of canker tissue for a definitive diagnosis.Contact:
Dr. Joseph Garvin DVM
Program Manager, Office of Laboratory Services
Virginia Dept. of Agriculture
804-692-0604
joseph.garvin@vdas.virginia.gov
Samples are sent to the Warrenton Regional Animal Health Lab:
272 Academy Hill Road
Warrenton, VA 20186
540-316-6543
![]() Click here for lab submission forms and to call the lab to set up payment/emailing test results to you.
Click here for lab submission forms and to call the lab to set up payment/emailing test results to you.
Why Need X-Rays of Foot?
A. Some horses may have infectious osteitis of the coffin bone, if the canker infection undermines the full sole thickness. This requires possible bone surgery, high powered antibiotics. Often in these, Naxcel is very helpful.
B. Some horses may have secondary laminitis on top of just the canker
C. Some horses may have bits of rock that jam up into/or under the sole and the horse will stay sore until removed.




; ?>/wp-content/themes/twentyten/img/NMImacLogo_150.jpg)